Our team of physical therapy experts have extensive experience working with athletes recovering from overuse and traumatic injuries, preventing injuries, and improving athletic performance.
We collaborate with your child's care team to develop personalized treatment plans to help them return to the playing field as quickly and safely as possible.
Our state-of-the-art facility is a motivating environment that allows close interaction between athletes and physical therapists. In addition to treatment, we provide ongoing education to athletes, families, coaches and physicians, and encourage active patient and family participation during the physical rehabilitation process.

Blood Flow Restriction Therapy
Patients recovering from an injury or surgery are often restricted from traditional strength training during early phases of their recovery, which can lead to atrophy and strength loss. Blood flow restriction (BFR) therapy is an alternative to traditional strength training during this time. BFR rehabilitation carefully applies pressure using a surgical grade tourniquet to the upper arm or leg while exercising, restricting blood flow in the veins. Using a personalized pressure, this can allow the patient to increase their strength and muscle mass with significantly lower loads then traditional strength training. Each training session tailors sets, repetitions, and resistance to the individual patient, in order to maximize their strength gains.
Concussion Therapy
A concussion is an injury to the brain that typically happens after a blow to the head or body. Patients may feel symptoms right after the blow or even a few days later. Symptoms can include headache, nausea and vomiting, dizziness and lightheadedness, sensitivity to light and sound, balance problems, and changes to vision. Patients may also notice a change in their sleep habits, difficulty focusing or concentrating, and emotional changes.
As part of our physical therapy services, we assess patients for concussion by testing mobility, strength, sensation and coordination, aerobic capacity, and evaluating balance and vision. We also complete a comprehensive assessment of the neck, since concussions can happen along with a whiplash injury to the neck. Based on this evaluation, we customize each patient’s treatment plan, which may include exercises for balance, vision, neck strength and mobility, and endurance. These exercises may be incorporated into a personalized rehabilitation plan, including follow-up visits and a home exercise program.
Toward the completion of the rehab program we start to add sport-specific exercises to see how the patient’s body tolerates the demands of their sport. We communicate with the patient’s doctor about this process, working as a team to help each athlete decide when they’re ready to get back in the game.
Dry Needling

Dry needling is a technique that uses a fine needle to treat underlying muscle trigger points, muscles, and connective tissues for the management of neuromusculoskeletal pain and movement impairments. It has been used to decrease pain, and reduce or restore impairments of body structure and function. Dry needling is often performed along with hands-on physical therapy techniques, therapeutic exercise, neuromuscular re-education, and functional retraining.
The use of dry needling can be very beneficial in the treatment of many orthopedic conditions. A skilled evaluation by one of our trained therapists determines if it’s an appropriate part of a patient’s treatment plan.
Interval Throwing Program
The Interval Throwing Program is used to gradually rebuild ball players’ throwing ability after an injury. Baseball and softball field players, pitchers, and catchers follow a multi-week treatment plan to regain range of motion, strength and endurance specific to the unique demands of baseball and softball.
The throwing program at Connecticut Children’s is designed to work in conjunction with each patient’s rehabilitation program and home exercise.
Instrument Assisted Soft Tissue Mobilization (IASTM)
Instrument Assisted Soft Tissue Mobilization (IASTM) is a non-invasive hand-held tool used by the clinician that glides over skin to help examine, locate, and treat inconsistencies in soft tissue and soft tissue restrictions. IASTM enables clinicians to effectively treat the adverse effects of scar tissue and fascial restrictions as well as improve and maintain optimal range of motion.
We often use IASTM for patients who have range of motion restrictions, pain, scar adhesions or difficulty recruiting muscle fibers. This can be used for diagnoses including tendinopathies, muscle strains, and ligament sprains of the IT band. Patients have reported improved outcomes with faster return to function and increased patient satisfaction.
Return to Sport Functional Test
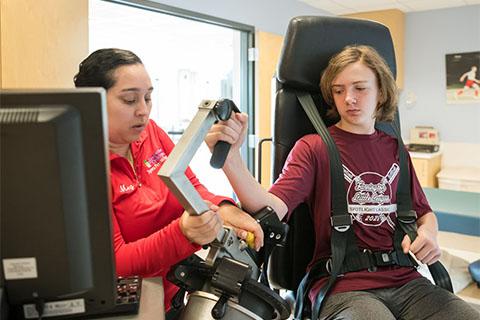
Returning to sports after surgery of the shoulder, elbow, hip, knee, or ankle can be a difficult transition for patients and their family. The specialists at Connecticut Children’s created a complete functional exam to test each patient’s readiness to return to sports. Each functional test assesses range of motion, strength and mobility to ensure a safe return to sports or activities.
An isokinetic test on our state-of-the-art HUMAC (Human Assessment Computer) compares a patient’s operative site to the opposite non-operative site to accurately gauge muscle strength.
Running Analysis Program
Connecticut Children’s two-dimensional running analysis is a comprehensive program consisting of multiple running trials on a Noraxon™ pressure treadmill. The Noraxon treadmill has the ability to capture the force generated from each foot upon landing, running cadence, symmetry of limbs, range of motion of each joint, and to record the runner from right, left and rear views. A physical therapist will collect and interpret this data in order to identify areas of need for the patient regarding injury rehabilitation, injury prevention or simply to improve running performance. Learn More
Transitional Therapy
Transitional therapy provides continued rehabilitation and training under professional guidance, monitoring the progress of rehabilitation after a patient is discharged from physical therapy. This program helps athletes return back to sports and includes sports performance training. Learn More
